Prostate cancer is a prevalent malignancy affecting men worldwide, with significant morbidity and mortality rates. Traditional treatments such as surgery, radiation, and chemotherapy have been the mainstay for managing this disease. However, a newer approach called immunotherapy is showing promise, especially for advanced cases. Immunotherapy is an exciting and rapidly evolving field in the fight against prostate cancer. This article will explore the latest advancements in immunotherapy for prostate cancer, explained in simple terms to ensure clarity and understanding.
Immunotherapy is a type of cancer treatment that harnesses the power of the body’s immune system to fight cancer cells. Unlike chemotherapy or radiation, which directly kill cancer cells, immunotherapy boosts the body’s natural defenses to recognize and attack cancer cells more effectively. This approach leverages the immune system’s ability to target and destroy cancer cells with greater precision.
Several types of immunotherapy are being used or investigated for the treatment of prostate cancer:
Think of cancer vaccines as a training program for your immune system. Normally, your immune system might not recognize cancer cells as a threat because they can look similar to normal cells. Cancer vaccines help by teaching your immune system to identify specific markers, or antigens, on the surface of cancer cells. Once trained, your immune system can seek out and attack these cancer cells more effectively.
Sipuleucel-T (Provenge): A Personalized Cancer Vaccine
One of the most well-known cancer vaccines for prostate cancer is Sipuleucel-T, also known as Provenge. This vaccine is unique because it is made specifically for each patient. Here’s how it works:
1. Collecting Immune Cells: First, some of your immune cells are collected from your blood. This process is similar to donating blood and takes a few hours.
2. Modifying the Cells: These collected cells are then sent to a lab, where they are exposed to a protein found on prostate cancer cells called prostatic acid phosphatase (PAP). This exposure trains the immune cells to recognize and attack prostate cancer cells.
3. Reintroducing the Cells: After the cells are modified, they are sent back to your doctor and infused into your body through a vein. This process is repeated two more times, two weeks apart, so you receive a total of three doses.
Immune checkpoint inhibitors represent a class of therapeutic agents designed to enhance the immune system’s ability to combat cancer. Under normal physiological conditions, the immune system possesses regulatory mechanisms, known as checkpoints, which serve to prevent excessive immune responses that could potentially harm the body’s own tissues. Cancer cells, however, can exploit these regulatory pathways by activating these checkpoints, thereby evading immune detection and destruction.
Checkpoint inhibitor medications function by targeting and inhibiting these regulatory pathways, specifically the interactions between checkpoint proteins and their ligands. This inhibition prevents the activation of the immune system’s “off switches,” thereby restoring the ability of immune cells, particularly T lymphocytes (T-cells), to recognize and attack cancer cells.
The mechanism of action of checkpoint inhibitors involves the removal of inhibitory signals that restrain the immune response against tumors. By blocking these inhibitory signals, checkpoint inhibitors enable a more robust and effective immune response. T-cells, which play a crucial role in the immune system’s ability to target and eliminate cancer cells, are thus activated and mobilized against the tumor.
The therapeutic application of checkpoint inhibitors offers a promising approach to cancer treatment, with the potential for durable responses and a reduced incidence of adverse effects compared to conventional therapies such as chemotherapy. This innovative strategy leverages the body’s innate defense mechanisms, offering a means to not only target and eliminate cancer cells but also to provide sustained protection against tumor progression and recurrence.
Here’s a brief overview of some key agents used in the treatment of prostate cancer:
Pembrolizumab (Keytruda)
• How It Works: Pembrolizumab targets the PD-1 (programmed death-1) receptor on T-cells, preventing cancer cells from using the PD-L1 protein to evade immune detection.
• Usage: Approved for use in various cancers, including prostate cancer with specific genetic mutations (mismatch repair deficiency or high microsatellite instability).
• Effectiveness: Shows antitumor activity in a subset of patients, particularly those with PD-L1-positive tumors or specific genetic markers.
• Side Effects: Common side effects include fatigue, rash, diarrhea, and immune-related adverse events like pneumonitis and colitis.
Ipilimumab (Yervoy)
• How It Works: Ipilimumab targets CTLA-4 (cytotoxic T-lymphocyte-associated protein 4), a checkpoint protein on T-cells that downregulates immune responses. By blocking CTLA-4, ipilimumab enhances T-cell activation and proliferation.
• Usage: Initially approved for melanoma, it has been studied in prostate cancer, particularly in combination with other treatments.
• Effectiveness: Has shown limited success as a monotherapy in prostate cancer but may be more effective when combined with other treatments like radiotherapy or other immunotherapies.
• Side Effects: Can cause severe immune-related side effects, including colitis, hepatitis, dermatitis, and endocrinopathies.
Nivolumab (Opdivo)
• How It Works: Nivolumab also targets the PD-1 receptor, similar to pembrolizumab, enhancing the immune system’s ability to detect and destroy cancer cells.
• Usage: Used in various cancers, including ongoing trials for prostate cancer, often in combination with other therapies.
• Effectiveness: Shows promise in combination therapies, particularly in patients with specific genetic mutations like BRCA1/2.
• Side Effects: Common side effects include fatigue, rash, musculoskeletal pain, and immune-related adverse events such as pneumonitis and colitis.
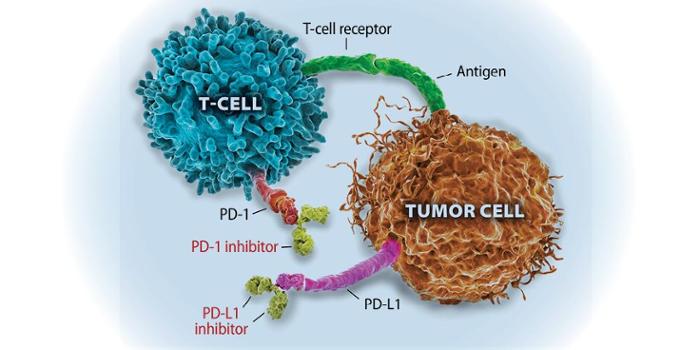
This image is taken from the upstate.edu
So in essence, these drugs don’t attack the cancer directly. Instead, they rally your own internal army to take on the fight, boosting your natural ability to combat the disease from within. For many patients, unleashing this innate cancer-fighting power can be a pivotal turning point in their treatment journey.
CAR T-cell therapy is an advanced treatment that enhances your immune system’s ability to recognize and attack cancer cells. Here’s how it works:
Your body naturally contains T-cells, a type of white blood cell that patrols for threats and eliminates them. However, cancer cells can sometimes evade detection by these T-cells.
In CAR T-cell therapy, your T-cells are collected and re-engineered in a laboratory to enhance their cancer-fighting capabilities. This process involves equipping the T-cells with chimeric antigen receptors (CARs), which are special proteins that allow the T-cells to identify cancer cells based on specific markers on their surface.
This modification essentially gives your T-cells a new ability to recognize and target cancer cells that were previously able to avoid detection. Once these enhanced CAR T-cells are infused back into your body, they seek out and destroy the cancer cells. Additionally, these CAR T-cells multiply, creating a growing population of cancer-fighting cells within your system.
This therapy has shown significant promise in treating certain types of blood cancers, particularly in cases where other treatments have failed. It represents a personalized and highly targeted approach to cancer treatment, leveraging the power of your own immune system to combat the disease.
This highly informative video is taken from the Peter MacCallum Cancer Centre
For many patients, unleashing the full potential of their immune system in this way can be the key to finally gaining ground against even the most stubborn cancers. It’s an ingenious approach that could open up new frontiers in the battle against this disease.
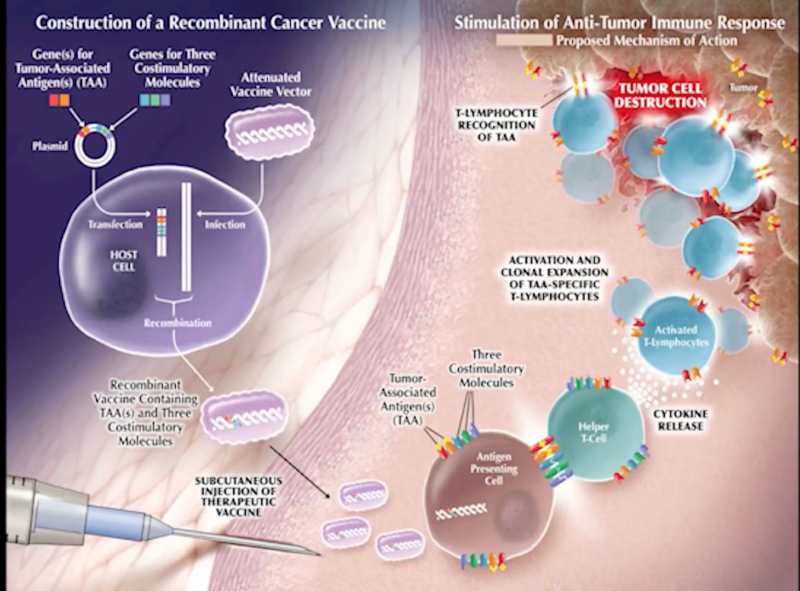
Prostate cancer Immunotherapy; This image is taken from grandroundsinurology.com
Immunotherapy has shown promise, particularly for advanced prostate cancer that has spread or does not respond to other treatments. However, its effectiveness can vary depending on factors such as the specific characteristics of the cancer and the patient’s overall health.
One of the challenges in using immunotherapy for prostate cancer is the tumor’s immunologically “cold” microenvironment, which means it has low levels of immune cell infiltration and a suppressive environment. This can make it difficult for the immune system to mount an effective response against the cancer cells.
Additionally, prostate cancer exhibits significant genetic diversity, which can affect the response to immunotherapy. Identifying specific genetic markers that predict treatment response is an ongoing area of research.
Despite the challenges, immunotherapy has shown promising results in improving overall survival for some patients with advanced prostate cancer. For example, the immunotherapy drug Sipuleucel-T (Provenge) has been shown to extend the lives of men with advanced prostate cancer by an average of several months.
In clinical trials, a small subset of patients (around 5%) treated with immunotherapy drugs like pembrolizumab (Keytruda) have experienced significant tumor shrinkage or even complete disappearance of their cancer. While the overall number of responders is small, the benefit can be long-lasting, with some patients remaining cancer-free for over two years.
It’s important to note that immunotherapy may not be suitable for everyone, and ongoing research is focused on identifying biomarkers and genetic markers that can predict which patients are most likely to benefit from these treatments.
While immunotherapy generally has fewer side effects than chemotherapy, it can still cause reactions.
Common Side Effects
Some of the most common side effects of immunotherapy for prostate cancer include:
• Fatigue and weakness
• Fever, chills, and flu-like symptoms
• Skin rash or itching
• Diarrhea or constipation
• Nausea and loss of appetite
• Joint or muscle pain
These side effects are generally mild to moderate and can often be managed with medications or by adjusting the treatment schedule.
Less Common but Serious Side Effects
In some cases, immunotherapy can cause the immune system to attack healthy organs and tissues, leading to more severe side effects known as immune-related adverse events (irAEs). These can affect various parts of the body, such as:
• Lungs (pneumonitis)
• Intestines (colitis)
• Liver (hepatitis)
• Endocrine glands (thyroid disorders, diabetes)
• Kidneys (nephritis)
• Nervous system (neuropathy, encephalitis)
While rare, these side effects can be serious and even life-threatening if not promptly recognized and treated.
It’s crucial to report any new or worsening symptoms to your healthcare team immediately. Early recognition and treatment of side effects can often prevent them from becoming severe. Depending on the severity, your doctor may recommend:
• Supportive care (e.g., medications for symptom relief)
• Temporarily stopping or adjusting the immunotherapy dose
• Using corticosteroids or other immunosuppressants to calm an overactive immune response
With proper monitoring and management, most side effects of immunotherapy can be controlled, allowing you to continue receiving this potentially life-extending treatment. Remember, your healthcare team is there to support you throughout your treatment journey. Don’t hesitate to discuss any concerns or questions you may have about managing side effects.
Immunotherapy is an exciting and rapidly evolving field in the fight against prostate cancer. While it may not be suitable for everyone, ongoing research and clinical trials are continuously improving our understanding and effectiveness of these treatments. Here are some promising areas of advancement:
Combination Therapies: A Powerful One-Two Punch
Researchers are exploring the potential of combining immunotherapy with other treatments like hormone therapy, chemotherapy, and radiation. The idea is that these different approaches can work together in a synergistic way, enhancing each other’s effectiveness. For example, hormone therapy has been shown to stimulate the immune system’s response against prostate cancer cells. When combined with immunotherapy, this “one-two punch” approach could potentially lead to better outcomes for patients with metastatic (spreading) prostate cancer. Early studies have shown promising results, with some patients experiencing significant tumor shrinkage or even complete disappearance of their cancer when treated with this combination approach.
New Targets and Innovative Approaches
Scientists are constantly on the lookout for new targets and innovative ways to harness the power of the immune system against prostate cancer. One area of focus is a protein called STEAP1, which is found on the surface of prostate cancer cells.
In preclinical studies (research done before human trials), targeting STEAP1 with a type of immunotherapy called CAR T-cell therapy has shown remarkable success in reducing tumor growth. CAR T-cell therapy involves genetically modifying a patient’s own immune cells to better recognize and attack cancer cells. While still in the early stages, these findings offer hope for the development of new and more effective immunotherapy treatments for prostate cancer.
Personalized Medicine: Tailoring Treatments for Better Results
Advances in genetic testing are enabling a more personalized approach to immunotherapy. By analyzing the specific genetic makeup of a patient’s cancer, doctors can tailor treatments to target those unique characteristics. This personalized approach has the potential to improve the chances of success and reduce the risk of side effects. It’s like having a custom-made treatment plan designed specifically for each individual patient. Researchers are working to identify genetic markers that can predict which patients are most likely to respond well to certain immunotherapies. This information can help guide treatment decisions and ensure that patients receive the most appropriate and effective therapies for their specific situation.
Clinical Trials: Paving the Way for New Treatments
Numerous clinical trials are currently underway, testing new immunotherapy drugs, combinations, and approaches for prostate cancer. These trials are crucial for determining the safety and effectiveness of new treatments and identifying which patients are most likely to benefit. By participating in clinical trials, patients not only gain access to cutting-edge therapies but also play a vital role in advancing medical research.
The data collected from these trials will help shape the future of prostate cancer treatment and potentially lead to life-saving breakthroughs. While there is still much work to be done, the future of immunotherapy for prostate cancer looks promising. With continued research, collaboration, and dedication, we may soon see more effective and personalized treatments that improve outcomes and quality of life for patients battling this disease.
More information about ongoing clinical trials can be found on the clinicaltrials.gov.
Immunotherapy represents a promising frontier in the treatment of prostate cancer, especially for those with advanced disease. While it may not be suitable for everyone, ongoing research and clinical trials are continually improving our understanding and effectiveness of these treatments. If you or a loved one is considering immunotherapy, it’s important to discuss with your doctor to understand the potential benefits and risks based on your specific situation.
Progression in immunotherapy for advanced prostate cancer – PMC.
Immunotherapy for Prostate Cancer.
Immunotherapy for Prostate Cancer: A Current Systematic Review.
Immunotherapy for Prostate Cancer.
Prostate cancer immunotherapy: a review of recent advancements.
Current Update on Prostate Cancer Immunotherapy.
What Are The Side Effects Of Prostate Cancer Treatment?
Prostate Cancer Immunotherapy: Effectiveness and Risks.
Immunotherapy for Prostate Cancer.
For Metastatic Prostate Cancer, Immunotherapy May Have Unexpected Potential.
Immunotherapy for Prostate Cancer.
Advances in Prostate Cancer Research.
Improving immunotherapy for advanced prostate cancer.
What’s New in Prostate Cancer Research?
Side Effects of Immunotherapy.
The article is taken from OncoDaily
About IMMONC
Immune Oncology Research Institute (IMMONC) is dedicated to advancing research aimed at preventing, treating, and ultimately curing cancer while making these innovations accessible to those who need them. If you're interested in joining our team, please feel free to contact us at [email protected] or at +374-41 310-048.