Breast cancer is one of the most common cancers affecting women worldwide. While traditional treatments like surgery, chemotherapy, and radiation therapy have been the mainstay of breast cancer management, recent years have seen a surge in the development and application of immunotherapy, a novel approach that harnesses the body’s own immune system to fight cancer cells. Immunotherapy has emerged as a promising treatment option, offering new hope for patients, particularly those with difficult-to-treat subtypes of breast cancer.
Breast cancer is a complex disease with various subtypes, each with its own unique characteristics and treatment responses. The most common subtypes are hormone receptor-positive (HR+), human epidermal growth factor receptor 2-positive (HER2+), and triple-negative breast cancer (TNBC). TNBC, which lacks expression of estrogen, progesterone, and HER2 receptors, is particularly challenging to treat and has a higher risk of recurrence and metastasis.
The immune system plays a crucial role in recognizing and eliminating cancer cells. However, cancer cells can develop mechanisms to evade immune surveillance, allowing them to grow and spread unchecked. Immunotherapy aims to overcome these evasion tactics by boosting the body’s immune response against cancer cells or by providing additional immune components to target and destroy the cancer cells more effectively.
This short video from the Rocky Mountain Cancer Centers explains how immunotherapy works
Immunotherapy has revolutionized the treatment landscape for breast cancer by leveraging the body’s immune system to target and destroy cancer cells. This approach includes various strategies, each with unique mechanisms and applications. Here, we delve into the primary types of immunotherapy used in breast cancer treatment, focusing on how they enhance the immune response against cancer cells.
Breast cancer immunotherapeutic options, this image is taken from actchealth.com
1. Immune Checkpoint Inhibitors (ICIs)
Immune checkpoint inhibitors are drugs that block proteins used by cancer cells to evade the immune system. These proteins, such as PD-1, PD-L1, and CTLA-4, act as “checkpoints” that can turn off immune responses. By inhibiting these checkpoints, ICIs can unleash the immune system’s ability to recognize and attack cancer cells more effectively.
• PD-1/PD-L1 Inhibitors: Drugs like pembrolizumab (Keytruda) and atezolizumab (Tecentriq) have shown promise, particularly in triple-negative breast cancer (TNBC) and HER2-positive breast cancer. These inhibitors have demonstrated improved overall survival in patients with PD-L1-positive tumors.
• CTLA-4 Inhibitors: Although less commonly used in breast cancer, CTLA-4 inhibitors like ipilimumab are being investigated in combination with PD-1/PD-L1 inhibitors to enhance therapeutic efficacy.
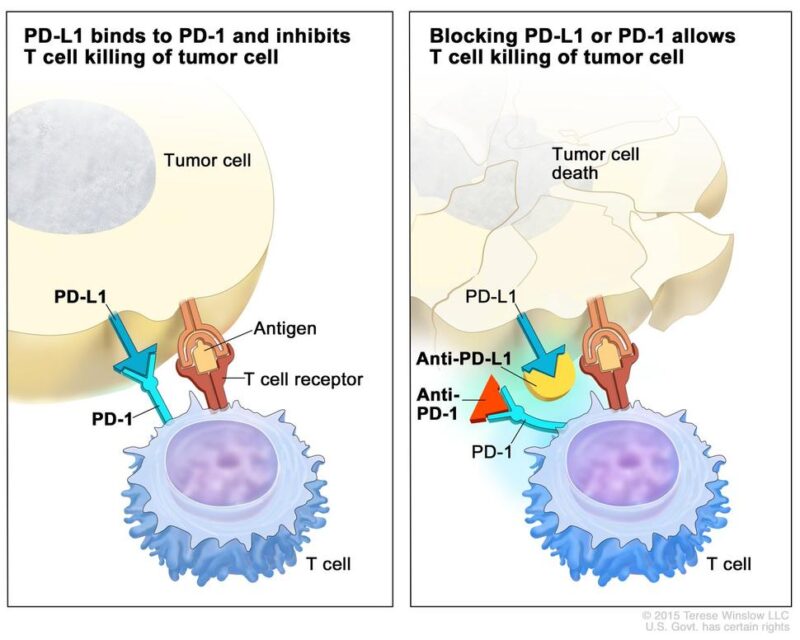
The image is taken from the cancer.gov (National Cancer Institute)
2. Monoclonal Antibodies
Monoclonal antibodies are laboratory-produced molecules that can bind to specific targets on cancer cells or immune cells. They can directly attack cancer cells, deliver cytotoxic agents, or modulate the immune system. Here’s how they help the immune system fight cancer:
• Direct Cell Killing: Certain antibodies can directly induce cancer cell death by disrupting vital cellular processes or triggering apoptosis (programmed cell death).
• Antibody-Dependent Cell-Mediated Cytotoxicity (ADCC): Antibodies bound to cancer cells can act as markers, allowing immune cells like natural killer (NK) cells to recognize and destroy the tagged cancer cells more effectively.
• Deliver Toxic Payloads: Antibodies can be conjugated with chemotherapeutic drugs, radioisotopes, or other cytotoxic agents, selectively delivering these toxic payloads to cancer cells while minimizing damage to healthy tissues.
Human antibodies (IgG) model; This picture is taken from news-medical.net
Examples of monoclonal antibodies targeting breast cancer cells include trastuzumab (Herceptin) and pertuzumab (Perjeta), which bind to the HER2 protein overexpressed in some breast cancers, leading to inhibition of tumor growth and increased cancer cell death.
3. Cancer Vaccines
Cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells by presenting specific tumor antigens. These vaccines can be used alone or in conjunction with other immunotherapies.
• HER2 Vaccines: Vaccines targeting the HER2 protein have shown promise in generating strong immune responses and improving survival in HER2-positive breast cancer patients. These vaccines are designed to prevent recurrence and treat existing cancer.
• DNA Vaccines: These vaccines use DNA to encode tumor antigens, which are then expressed by the patient’s cells, eliciting an immune response. DNA vaccines targeting HER2 have shown encouraging results in clinical trials.
4. Adoptive Cell Therapy (ACT)
Adoptive cell therapy involves collecting and modifying a patient’s immune cells to enhance their ability to fight cancer. This approach includes several strategies:
• Tumor-Infiltrating Lymphocytes (TILs): TIL therapy involves extracting lymphocytes from a tumor, expanding them in the lab, and reinfusing them into the patient. This method has shown promise in various cancers, including breast cancer.
• Chimeric Antigen Receptor (CAR) T-Cell Therapy: CAR T-cell therapy involves genetically engineering T cells to express receptors that specifically target cancer cells. This approach has been successful in blood cancers and is being explored for solid tumors like breast cancer.
• Engineered T Cell Receptor (TCR) Therapy: This therapy involves modifying T cells to express receptors that recognize specific cancer antigens, enhancing their ability to target and kill cancer cells.
This video from the Peter MacCallum Cancer Centre gives valuable and interesting information regarding CAR-T Cells and CAR-T Cell therapy
5. Oncolytic Virus Therapy
Oncolytic viruses are engineered to selectively infect and kill cancer cells while stimulating an immune response against the tumor.
• Oncolytic Viruses: These viruses can be used alone or in combination with other immunotherapies to enhance their efficacy. They represent a novel approach to cancer treatment, with ongoing research exploring their potential in breast cancer
6. Combination Therapies
Combining different immunotherapy approaches or combining immunotherapy with traditional treatments like chemotherapy, radiation, or targeted therapies can enhance the overall effectiveness of cancer treatment.
• Combination with Chemotherapy: Combining ICIs with chemotherapy has shown improved outcomes in TNBC and other breast cancer subtypes.
• Combination with Targeted Therapies: Combining monoclonal antibodies with ICIs or other targeted agents can enhance the immune response and improve treatment efficacy.
While immunotherapy has shown significant promise, several challenges remain, including identifying predictive biomarkers, managing immune-related adverse events, and overcoming resistance mechanisms. Ongoing research and clinical trials are focused on addressing these challenges and expanding the use of immunotherapy in breast cancer treatment.
In conclusion, immunotherapy represents a transformative approach in the fight against breast cancer, offering new hope for patients with difficult-to-treat subtypes. Continued advancements in this field hold the potential to improve outcomes and provide more personalized and effective treatment options for breast cancer patients.
Immunotherapy has significantly advanced the treatment landscape for breast cancer, particularly for aggressive subtypes like triple-negative breast cancer (TNBC). Here, we summarize the recent achievements and ongoing research efforts in this field, highlighting FDA approvals, biomarker development, combination strategies, and novel immunotherapy approaches.
FDA Approvals
Atezolizumab (Tecentriq) and Nab-Paclitaxel (Abraxane):
• Approval for Metastatic TNBC: In March 2019, the FDA granted accelerated approval to the combination of atezolizumab and nab-paclitaxel for the treatment of PD-L1-positive metastatic TNBC.
• Withdrawal of Indication: Despite the initial approval, the indication for atezolizumab in combination with nab-paclitaxel was voluntarily withdrawn by Roche in August 2021 due to the failure of the IMpassion131 trial to meet its primary endpoint of improved PFS.
Pembrolizumab (Keytruda):
• Approval for Early-Stage TNBC: On July 26, 2021, the FDA approved pembrolizumab in combination with chemotherapy for the neoadjuvant (before the surgery) treatment of high-risk, early-stage TNBC, followed by continued use as a single agent for adjuvant treatment after surgery.
Approval for Metastatic TNBC: Pembrolizumab also received accelerated approval for use in combination with chemotherapy for patients with locally recurrent unresectable or metastatic TNBC whose tumors express PD-L1.
Biomarker Development
Identifying predictive biomarkers is crucial for optimizing immunotherapy in breast cancer. Several biomarkers are being actively researched:
• PD-L1 Expression: PD-L1 expression on tumor cells and tumor-infiltrating immune cells is a key biomarker for predicting response to immune checkpoint inhibitors (ICIs). However, its predictive value can vary between early and metastatic settings.
• Tumor Mutational Burden (TMB): High TMB is associated with a higher likelihood of response to ICIs, as it indicates a greater number of neoantigens that can be recognized by the immune system.
• Tumor-Infiltrating Lymphocytes (TILs): The presence of TILs in the tumor microenvironment is another potential biomarker for predicting response to immunotherapy. Higher levels of TILs are generally associated with better outcomes.
Combination Strategies
Combining immunotherapy with other treatment modalities is a promising approach to enhance the immune response and overcome resistance mechanisms. Several combination strategies are under investigation:
• Chemotherapy and ICIs: Combining ICIs with chemotherapy has shown improved outcomes in TNBC and other breast cancer subtypes. For example, the combination of pembrolizumab with chemotherapy has been effective in both early-stage and metastatic TNBC.
• Radiotherapy and ICIs: Radiotherapy can enhance the immunogenicity of tumors by promoting antigen presentation and stimulating an anti-tumor immune response. Combining radiotherapy with ICIs is being explored in clinical trials to improve therapeutic efficacy and reduce recurrence.
• Targeted Therapies and ICIs: Combining monoclonal antibodies with ICIs or other targeted agents can enhance the immune response and improve treatment efficacy. For instance, combining trastuzumab with pembrolizumab has shown potential in HER2-positive breast cancer.
Novel Immunotherapy Approaches
Researchers are exploring new immunotherapy strategies to provide additional treatment options for breast cancer patients:
• Bispecific Antibodies: These engineered antibodies can simultaneously bind to two different targets, such as a tumor antigen and an immune cell receptor, facilitating the recruitment and activation of immune cells against cancer cells. Bispecific antibodies are being investigated in clinical trials for their potential to enhance anti-tumor immunity.
• Oncolytic Viruses: Oncolytic viruses are designed to selectively infect and kill cancer cells while stimulating an immune response against the tumor. This approach is being explored in combination with other immunotherapies to enhance their efficacy.
• Cancer Vaccines: Vaccines targeting specific tumor antigens aim to stimulate the immune system to recognize and attack cancer cells. HER2 vaccines and DNA vaccines are among the promising candidates being evaluated in clinical trials.
• Chimeric Antigen Receptor (CAR) T-Cell Therapy: CAR T-cell therapy involves genetically engineering T cells to express receptors that specifically target cancer cells. This approach has been successful in blood cancers and is being explored for solid tumors like breast cancer.
Immunotherapy, particularly immune checkpoint inhibitors (ICIs), has emerged as a promising treatment approach for breast cancer, especially for the triple-negative subtype. However, like any cancer treatment, immunotherapy can cause adverse effects and toxicities, which are collectively known as immune-related adverse events (irAEs). Here are some key points about the adverse effects and toxicities associated with immunotherapy in breast cancer:
1. Immune-related adverse events (irAEs):
• irAEs are a unique set of side effects caused by the overstimulation of the immune system, leading to autoimmune-like reactions against healthy tissues and organs.
• Common irAEs include skin rashes, colitis, hepatitis, endocrinopathies (thyroid dysfunction, adrenal insufficiency), pneumonitis, and neurological toxicities.
• The incidence and severity of irAEs can vary depending on the specific ICI used, the combination of therapies, and individual patient factors.
2. Incidence and severity of irAEs in breast cancer:
• In clinical trials evaluating ICIs for breast cancer, the reported incidence of any-grade irAEs ranges from approximately 20% to 40%.
• Severe (grade 3 or higher) irAEs occur in around 5% to 15% of patients.
• The most common irAEs observed in breast cancer trials include thyroid dysfunction, skin rashes, hepatitis, pneumonitis, and colitis
3. Risk factors for irAEs:
• Combination therapy with chemotherapy or other immunotherapies increases the risk of irAEs compared to ICI monotherapy.
• Certain patient factors, such as autoimmune disorders, may predispose individuals to a higher risk of developing irAEs.
• Biomarkers like tumor mutational burden (TMB) and PD-L1 expression may help identify patients at higher risk for irAEs, but more research is needed.
4. Management of irAEs:
• Early recognition and prompt management of irAEs are crucial to prevent potentially life-threatening complications.
• Treatment typically involves withholding or discontinuing the ICI, administering corticosteroids or other immunosuppressive agents, and providing supportive care.
• Multidisciplinary collaboration with specialists (e.g., endocrinologists, gastroenterologists, pulmonologists) is often required for managing organ-specific irAEs.
5. Impact on treatment outcomes:
• While irAEs can be challenging to manage, some studies suggest that their occurrence may be associated with improved treatment outcomes, potentially indicating a more robust immune response against the tumor.
• However, severe irAEs may necessitate treatment discontinuation, potentially limiting the therapeutic benefit.
Healthcare providers and patients need to be aware of the potential adverse effects and toxicities associated with immunotherapy in breast cancer. Close monitoring, early recognition, and prompt management of irAEs are crucial for ensuring patient safety and optimizing treatment outcomes.
The prognosis for breast cancer patients receiving immunotherapy depends on various factors, including the cancer subtype, stage, and specific treatment regimen. While immunotherapy has shown promising results, particularly in TNBC and HER2-positive breast cancer, it is important to note that not all patients will respond to these treatments.
Ongoing research efforts are focused on improving the efficacy of immunotherapy, identifying predictive biomarkers, and developing novel combination strategies to overcome resistance mechanisms. Additionally, researchers are exploring the potential of immunotherapy in earlier stages of breast cancer, intending to prevent recurrence and improve long-term outcomes.
While immunotherapy represents a significant advancement in breast cancer treatment, it is important to recognize that it may not be suitable or effective for all patients. In such cases, alternative and complementary approaches may be considered:
1. Traditional Treatments: Surgery, chemotherapy, radiation therapy, and targeted therapies (e.g., endocrine therapy, HER2-targeted agents) remain essential components of breast cancer management and may be used in combination with or as alternatives to immunotherapy.
2. Clinical Trials: Participation in clinical trials investigating novel treatments, combination strategies, or alternative immunotherapy approaches may provide access to cutting-edge therapies and contribute to the advancement of breast cancer research.
3. Supportive Care: Palliative care, complementary therapies (e.g., acupuncture, massage, mindfulness practices), and lifestyle modifications (e.g., diet, exercise) can help manage symptoms, improve quality of life, and support overall well-being during and after cancer treatment.
4. Integrative Approach: A comprehensive, integrative approach that combines conventional treatments, immunotherapy (when appropriate), and supportive care measures may offer the best outcomes for breast cancer patients.
Immunotherapy has emerged as a promising treatment option for breast cancer, offering new hope for patients, particularly those with difficult-to-treat subtypes like TNBC. While significant progress has been made, ongoing research efforts are focused on improving efficacy, identifying predictive biomarkers, and developing novel combination strategies to overcome resistance mechanisms. Patients need to have open and honest discussions with their healthcare team about the potential benefits, risks, and side effects of immunotherapy, as well as alternative and complementary approaches.
By staying informed and actively participating in treatment decisions, patients can play a crucial role in their cancer journey and contribute to the advancement of breast cancer research. Remember, immunotherapy is a rapidly evolving field, and new developments and breakthroughs are constantly emerging. With continued research and collaboration among scientists, clinicians, and patients, the future of breast cancer treatment holds great promise.
Pembrolizumab for early triple-negative breast cancer. New England Journal of Medicine
Biomarkers for breast cancer immunotherapy: PD-L1, TILs, and TMB. PubMed (2021).
Effective Combinations of Immunotherapy and Radiotherapy for Cancer Treatment. PMC (2022).
The article is taken from OncoDaily
About IMMONC
Immune Oncology Research Institute (IMMONC) is dedicated to advancing research aimed at preventing, treating, and ultimately curing cancer while making these innovations accessible to those who need them. If you're interested in joining our team, please feel free to contact us at [email protected] or at +374-41 310-048.