Head and neck cancer refers to a diverse group of malignancies that originate in the squamous cells lining the mucosal surfaces of the head and neck region. These cancers can develop in various anatomical sites, including the oral cavity, pharynx, larynx, nasal cavity, and salivary glands. The majority of head and neck cancers are squamous cell carcinomas (HNSCC), which account for approximately 90% of cases.
Globally, head and neck cancer is the seventh most common cancer, with more than 660,000 new cases and 325,000 deaths reported annually. The incidence of head and neck cancer is increasing, particularly driven by a rise in oropharyngeal cancers linked to human papillomavirus (HPV) infection. This trend is observed despite a decline in smoking rates, which historically has been a major risk factor for these cancers. Other significant risk factors include alcohol consumption, betel quid chewing (especially in Southeast Asia), and Epstein-Barr virus (EBV) infection, particularly in nasopharyngeal cancer. The burden of head and neck cancer varies significantly by geographic region and demographic characteristics, with higher incidence rates observed in men, older adults, and individuals of lower socioeconomic status.
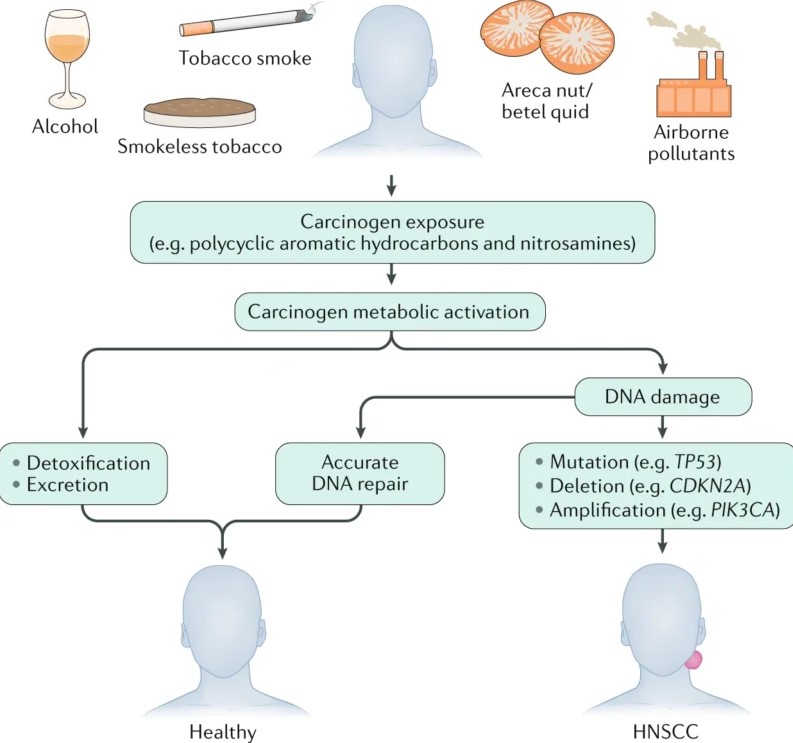
Development of carcinogen-associated, HPV-negative HNSCC. The image is taken from a paper by Johnson et al. (2020).
The treatment of head and neck cancers is multifaceted, involving a combination of surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The choice of treatment depends on various factors, including the cancer’s location, stage, and the patient’s overall health and preferences. Here are the primary treatment options:
Surgery
Often the first-line treatment for localized head and neck cancer, surgery aims to remove the tumor and some surrounding healthy tissue. Types of surgery include:
• Tumor Resection: Involves the surgical removal of the tumor along with a margin of healthy tissue to ensure complete excision.
• Neck Dissection: Removal of lymph nodes in the neck if cancer has spread.
• Reconstructive Surgery: Restores appearance and function after tumor removal.
Radiation Therapy
• External Beam Radiation Therapy: Uses high-energy rays to destroy cancer cells. Techniques like Intensity-modulated radiation therapy precisely target the tumor while sparing healthy tissue, reducing side effects.
• Brachytherapy: Involves placing radioactive sources directly into or near the tumor, providing a high radiation dose to the cancer while minimizing exposure to surrounding healthy tissues
Chemotherapy
• Cisplatin and Carboplatin: Commonly used drugs that kill cancer cells or stop them from growing. Chemotherapy can be used alone or in combination with radiation therapy (chemoradiation) for advanced cancers.
• Neoadjuvant Chemotherapy: Administered before surgery or radiation to shrink tumors, making them easier to treat.
• Adjuvant Chemotherapy: Given after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence.
Targeted Therapy
• Cetuximab (Erbitux): Targets the epidermal growth factor receptor (EGFR), which is often overexpressed in head and neck cancer. By inhibiting EGFR, cetuximab can slow tumor growth and enhance the effects of radiation therapy.
Immunotherapy has emerged as a groundbreaking treatment modality for various cancers, including head and neck cancers. Unlike traditional treatments such as chemotherapy and radiation, which directly target cancer cells, immunotherapy leverages the body’s immune system to recognize and combat cancer cells. This approach has shown promise in treating recurrent and metastatic head and neck squamous cell carcinoma, which often presents significant treatment challenges due to its aggressive nature and tendency to recur after initial treatment.
The immune system plays a crucial role in identifying and eliminating abnormal cells, including cancer cells. However, cancer cells can develop mechanisms to evade immune detection, such as expressing proteins that inhibit immune responses. Immunotherapy aims to overcome these evasion tactics by enhancing the immune system’s ability to detect and destroy cancer cells. This is achieved through various strategies, including immune checkpoint inhibitors, adoptive cell transfer, and therapeutic vaccines, each targeting different aspects of the immune response.
Head and neck cancers, particularly HNSCC, are known for their complex tumor microenvironment, which includes a variety of immune cells, stromal cells, and cytokines. This environment can either support or inhibit tumor growth and metastasis. Immunotherapy works by modulating this microenvironment to favor an anti-tumor response. For instance, immune checkpoint inhibitors block proteins that suppress immune activity, thereby allowing T cells to attack cancer cells more effectively.
One of the primary targets in immunotherapy for head and neck cancer is the PD-1/PD-L1 pathway. PD-1 is a protein on the surface of T cells that, when bound to its ligand PD-L1 on cancer cells, inhibits T cell activity. By blocking this interaction, drugs like pembrolizumab (Keytruda) and nivolumab (Opdivo) can enhance the immune system’s ability to fight cancer. These drugs have shown significant efficacy in clinical trials, leading to their approval for treating recurrent or metastatic HNSCC.
More information about completed and ongoing clinical trials for head and neck cancer immunotherapy can be found here – clinicaltrials.gov.
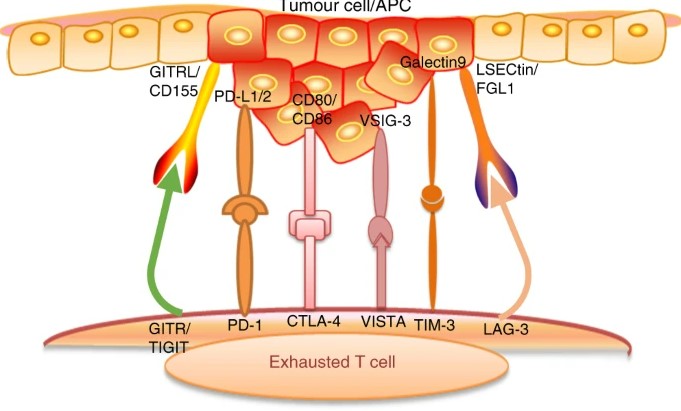
In head and neck squamous cell carcinoma, several coinhibitory pathways impede T-cell activation during carcinogenesis. Tumor cells or antigen-presenting cells express specific ligands, such as PD-L1/2, CD80/CD86, galectin 9, LSECtin/FGL1, CD155/GITRL, and VSIG-3. These ligands bind to receptors on T cells, including PD-1, CTLA-4, TIM-3, LAG-3, TIGIT, GITR, and VISTA, thereby suppressing T cell activation and hindering their anti-tumor function. The image is taken from a paper by Mei et al. (2020).
Several types of immunotherapy are currently used or being investigated for the treatment of head and neck cancers:
• Immune Checkpoint Inhibitors: These drugs block proteins that prevent the immune system from attacking cancer cells. The most common targets are PD-1 and PD-L1.
• Adoptive Cell Transfer: This involves collecting and modifying a patient’s T cells to enhance their ability to fight cancer, then reintroducing them into the patient. One example is CAR T-cell therapy, where T cells are engineered to express chimeric antigen receptors (CARs) that target specific proteins on cancer cells.
• Therapeutic Vaccines: These vaccines are designed to stimulate the immune system to attack cancer cells by targeting specific antigens present on the tumor. For example, vaccines targeting HPV-related antigens are being developed for HPV-associated HNSCC.
• Oncolytic Virus Therapy: This approach uses genetically modified viruses to infect and kill cancer cells while stimulating an immune response. The viruses are designed to selectively target cancer cells, sparing normal cells.
Each of these immunotherapy strategies offers unique advantages and has the potential to improve outcomes for patients with head and neck cancers. Ongoing research and clinical trials continue to explore new combinations and applications of these therapies to enhance their efficacy and expand their use in different stages of the disease.
Several immunotherapy drugs have been approved for the treatment of head and neck cancers, particularly for recurrent or metastatic squamous cell carcinoma. These drugs primarily include immune checkpoint inhibitors that target the PD-1/PD-L1 pathway.
Approved Drugs
• Pembrolizumab (Keytruda): Targets PD-1, blocking its interaction with PD-L1 and PD-L2, thereby enhancing the immune response against cancer cells. Approved for use in patients with recurrent or metastatic head and neck cancer, either as monotherapy or in combination with chemotherapy.
• Nivolumab (Opdivo): Another PD-1 inhibitor that works similarly to pembrolizumab. It is approved for patients with recurrent or metastatic HNC who have progressed on or after platinum-based chemotherapy.
• Durvalumab (Imfinzi): Targets PD-L1, blocking its interaction with PD-1 and B7.1, enhancing the immune response. It is being investigated in combination with other therapies for head and neck cancer.
• Atezolizumab (Tecentriq): A PD-L1 inhibitor that is being studied in clinical trials for its efficacy in head and neck cancer.
Benefits of Immunotherapy for Head and Neck Cancer
Immunotherapy has revolutionized the treatment landscape for head and neck cancers, particularly for patients with recurrent or metastatic disease. The primary benefits of immunotherapy include:
• Long-lasting Responses: Immunotherapy can lead to durable responses, with some patients experiencing prolonged periods of cancer control. This is particularly significant for patients with advanced head and neck cancers, where traditional treatments often fail to provide long-term benefits.
• Improved Survival Rates: Clinical trials have demonstrated that immunotherapy can extend overall survival in patients with head and neck cancers. For instance, the use of immune checkpoint inhibitors like pembrolizumab and nivolumab has been associated with significant survival benefits compared to standard chemotherapy.
• Enhanced Quality of Life: Compared to traditional chemotherapy, immunotherapy often has a more favorable side effect profile, leading to a better quality of life for patients. This is crucial for head and neck cancer patients, who may already be dealing with significant functional impairments due to their disease and its treatment.
While immunotherapy offers substantial benefits, it can also cause a range of side effects, primarily due to the activation of the immune system. These side effects, known as immune-related adverse events (irAEs), can affect various organs and systems in the body. The severity of these side effects can vary from mild to life-threatening.
Common Side Effects
• Fatigue: Fatigue is the most common side effect of immunotherapy. It is usually mild but can be severe in some cases. Patients may feel extremely tired and lack energy, which can impact their daily activities.
• Skin Reactions: Skin-related side effects, such as rash, itching, and vitiligo, are common. These reactions are usually mild but can be bothersome for patients.
• Gastrointestinal Issues: Diarrhea, nausea, vomiting, and loss of appetite are frequent gastrointestinal side effects. These can range from mild to severe and may require medical intervention.
• Endocrine Disorders: Immunotherapy can affect the endocrine system, leading to conditions such as hypothyroidism, hyperthyroidism, and adrenal insufficiency. These conditions often require long-term hormone replacement therapy.
• Respiratory Issues: Shortness of breath and cough are common respiratory side effects. In severe cases, patients may develop pneumonitis, an inflammation of the lung tissue.
• Liver Toxicity: Elevated liver enzymes and hepatitis can occur, indicating liver inflammation or damage. This requires close monitoring and may necessitate treatment adjustments.
• Neurological Symptoms: Neurological side effects, such as headaches, dizziness, and peripheral neuropathy, can occur. These are less common but can be severe.
Effective management of immunotherapy side effects is crucial to ensure patient safety and the continuation of treatment. The approach to managing side effects depends on their severity and the specific symptoms experienced by the patient.
General Management Strategies
• Regular Monitoring: Patients undergoing immunotherapy should have regular check-ups and blood tests to monitor for potential side effects. Early detection is key to managing irAEs effectively.
• Patient Education: Educating patients about the potential side effects of immunotherapy and the importance of reporting any new or worsening symptoms promptly is essential. This helps in early identification and management of irAEs.
• Symptom Management: Mild side effects can often be managed with supportive care measures, such as rest, hydration, and over-the-counter medications. For example, anti-nausea medications can help manage gastrointestinal symptoms, and topical treatments can alleviate skin reactions.
Specific Management Strategies
• Fatigue: Encourage patients to rest and pace their activities. Light exercise, such as walking, can help improve energy levels. Nutritional support, including a balanced diet and adequate hydration, is also important.
• Skin Reactions: Use gentle skin care products and avoid harsh soaps and lotions. Topical corticosteroids may be prescribed for more severe rashes. Patients should avoid sun exposure and use sunscreen to protect their skin.
• Gastrointestinal Issues: Dietary modifications, such as eating small, frequent meals and avoiding spicy or fatty foods, can help manage nausea and diarrhea. Anti-diarrheal medications and anti-nausea drugs may be prescribed as needed.
• Endocrine Disorders: Hormone replacement therapy is often required for conditions like hypothyroidism and adrenal insufficiency. Regular monitoring of hormone levels and adjusting medication dosages as needed is crucial.
• Respiratory Issues: Patients with symptoms of pneumonitis should be evaluated promptly. Treatment typically involves corticosteroids to reduce lung inflammation.
• Liver Toxicity: Regular monitoring of liver function tests is essential. If liver enzymes are elevated, corticosteroids may be prescribed to reduce inflammation.
• Neurological Symptoms: Neurological side effects require prompt evaluation by a neurologist. Treatment may involve corticosteroids and other immunosuppressive therapies. Close monitoring of neurological function is essential.
In this video prepared by the American Society of Clinical Oncology, the side effects of immunotherapy are discussed.
Immunotherapy for head and neck cancer: Present and future – Critical Reviews in Oncology/Hematology
Immunotherapy drug approved for head and neck cancer – Cancer Research UK
Immunotherapy in Head and Neck Cancer When, How, and Why? – Biomedicines
National Cancer Institute – cancer.org
American Society of Clinical Oncology – asco.org
The article is taken from OncoDaily.
About IMMONC
Immune Oncology Research Institute (IMMONC) is dedicated to advancing research aimed at preventing, treating, and ultimately curing cancer while making these innovations accessible to those who need them. If you're interested in joining our team, please feel free to contact us at [email protected] or at +374-41 310-048.