Immunotherapy represents a paradigm shift in the treatment of ovarian cancer, leveraging the body’s immune system to combat cancer cells. Unlike traditional treatments such as chemotherapy and radiation, which directly target and kill cancer cells, immunotherapy works by enhancing the immune system’s ability to recognize and destroy these cells. This approach is particularly promising for ovarian cancer, which is often diagnosed at an advanced stage and has a high rate of recurrence.
The immune system is a complex network of cells, tissues, and organs that work together to defend the body against harmful invaders, including cancer cells. However, cancer cells can evade the immune system by exploiting certain mechanisms, such as immune checkpoints. These checkpoints are proteins on immune cells that need to be activated (or deactivated) to initiate an immune response. Cancer cells can manipulate these checkpoints to avoid being attacked by the immune system. Immunotherapy drugs, such as immune checkpoint inhibitors, work by blocking these proteins, thereby allowing the immune system to recognize and attack cancer cells more effectively.
In ovarian cancer, immunotherapy is still an emerging field, with various strategies being explored. These include immune checkpoint inhibitors, cancer vaccines, adoptive cell transfer, and oncolytic viruses. Each of these approaches aims to boost the immune system’s ability to fight cancer in different ways. For instance, immune checkpoint inhibitors block proteins that prevent T cells from attacking cancer cells, while cancer vaccines stimulate the immune system to recognize and target specific cancer antigens. Adoptive cell transfer involves modifying a patient’s T cells to enhance their cancer-fighting capabilities, and oncolytic viruses are engineered to selectively infect and kill cancer cells.
Watch this short video about ovarian cancer by Cancer Research UK.
The landscape of immunotherapy for ovarian cancer is diverse, encompassing several types of drugs and treatment modalities. Here, we provide a comprehensive overview of the most prominent types of immunotherapy drugs used in the treatment of ovarian cancer.
Immune Checkpoint Inhibitors
Immune checkpoint inhibitors are the most widely studied and used form of immunotherapy in ovarian cancer. These drugs work by blocking checkpoint proteins, such as PD-1, PD-L1, and CTLA-4, which cancer cells use to evade the immune system. By inhibiting these proteins, immune checkpoint inhibitors enable T cells to recognize and attack cancer cells more effectively.
• Pembrolizumab (Keytruda): This drug targets the PD-1 protein on T cells, preventing it from binding to PD-L1 on cancer cells. Pembrolizumab has shown promise in treating advanced ovarian cancer, particularly in patients with high microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR).
• Nivolumab (Opdivo): Another PD-1 inhibitor, nivolumab has been studied in combination with other therapies for ovarian cancer. It has shown potential in improving response rates and overall survival in some patients.
• Atezolizumab (Tecentriq): This PD-L1 inhibitor has been evaluated in clinical trials for ovarian cancer, often in combination with other treatments such as chemotherapy or targeted therapy.
• Ipilimumab (Yervoy): Targeting the CTLA-4 protein, ipilimumab has been used in combination with other immunotherapies to enhance the immune response against ovarian cancer cells.
Cancer Vaccines
Cancer vaccines are designed to stimulate the immune system to recognize and attack specific antigens found on cancer cells. These vaccines can be made from a patient’s own tumor cells or synthetic versions of cancer antigens.
• Dendritic Cell Vaccines: These vaccines involve extracting dendritic cells from a patient, loading them with cancer antigens, and then reintroducing them into the patient to stimulate an immune response. Research is ongoing to develop effective dendritic cell vaccines for ovarian cancer.
• Peptide Vaccines: These vaccines use short sequences of amino acids (peptides) that mimic antigens found on cancer cells. The goal is to train the immune system to recognize and attack cells expressing these antigens.
Adoptive Cell Transfer
Adoptive cell transfer (ACT) involves collecting and modifying a patient’s T cells to enhance their ability to fight cancer. These modified T cells are then expanded in the laboratory and infused back into the patient.
• Chimeric Antigen Receptor (CAR) T-Cell Therapy: This form of ACT involves genetically engineering T cells to express receptors that specifically target cancer cells. CAR T-cell therapy has shown promise in treating certain types of ovarian cancer, particularly those with specific antigen expressions such as Mucin 16 and mesothelin.
• Tumor-Infiltrating Lymphocytes (TILs): TIL therapy involves isolating T cells that have naturally infiltrated a tumor, expanding them in the lab, and then reinfusing them into the patient. This approach aims to boost the body’s natural immune response to cancer.
Oncolytic Viruses
Oncolytic viruses are genetically engineered viruses that selectively infect and kill cancer cells. These viruses can also stimulate an immune response against the tumor.
• Talimogene Laherparepvec (T-VEC): This oncolytic virus, derived from the herpes simplex virus, has been studied in combination with other immunotherapies for ovarian cancer. It works by infecting and lysing cancer cells, releasing tumor antigens that stimulate an immune response.
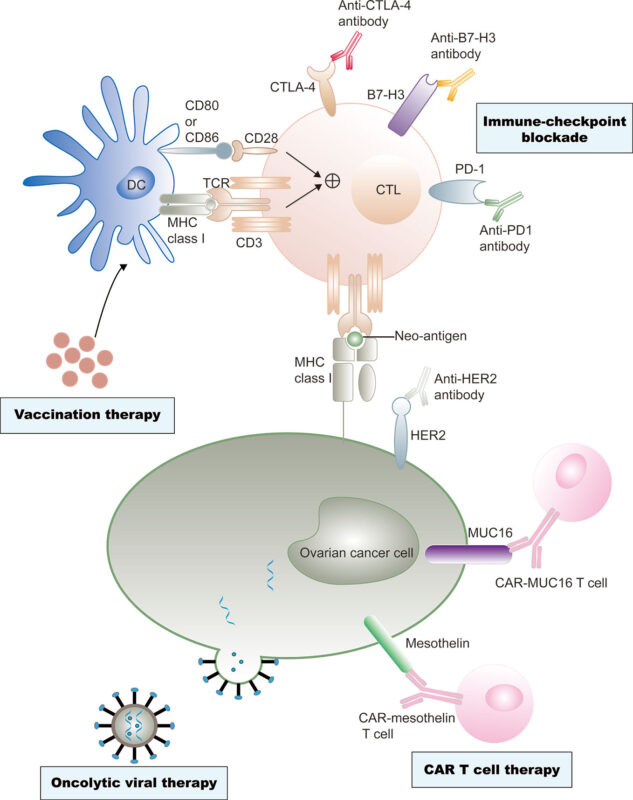
Current immunotherapy treatments of ovarian cancer. Image source: Yang et al. (2020).
Immunotherapy offers a novel approach to treating ovarian cancer, but it is essential to compare it with traditional treatment options to understand its benefits and limitations fully.
Surgery
Surgery is often the first line of treatment for ovarian cancer, aiming to remove as much of the tumor as possible. The extent of surgery depends on the stage and spread of the cancer. Common procedures include unilateral or bilateral salpingo-oophorectomy (removal of one or both ovaries), hysterectomy (removal of the uterus), and omentectomy (removal of the omentum).
Chemotherapy
Chemotherapy uses drugs to kill rapidly dividing cancer cells. It is typically administered after surgery to eliminate any remaining cancer cells and reduce the risk of recurrence. Common chemotherapy drugs for ovarian cancer include paclitaxel and carboplatin. While effective, chemotherapy can cause significant side effects, such as hair loss, nausea, and fatigue.
Targeted Therapy
Targeted therapy involves drugs that specifically target molecular pathways involved in cancer growth and survival. These therapies are designed to be more selective than chemotherapy, potentially reducing side effects.
• PARP Inhibitors: These drugs, such as olaparib and niraparib, target the DNA repair pathways in cancer cells, making it difficult for them to repair damage and survive. PARP inhibitors have shown significant efficacy in patients with BRCA1 or BRCA2 mutations.
• Angiogenesis Inhibitors: Bevacizumab is an example of an angiogenesis inhibitor that works by cutting off the blood supply to tumors, thereby inhibiting their growth. It is often used in combination with chemotherapy for recurrent ovarian cancer.
Hormone Therapy
Hormone therapy is used to treat ovarian cancers that are sensitive to hormones such as estrogen. This treatment involves drugs that block the effects of hormones on cancer cells, slowing their growth. Hormone therapy is less commonly used for ovarian cancer compared to other treatments.
In a study published in NEJM, maintenance therapy with olaparib significantly improved progression-free survival in women with newly diagnosed advanced ovarian cancer and a BRCA1/2 mutation, reducing the risk of disease progression or death by 70% compared to placebo.
Immunotherapy can cause a range of side effects, which can vary depending on the type of drug used, the dose, and the individual patient’s response. It is crucial for patients to be aware of these potential side effects and to communicate any symptoms to their healthcare team promptly.
Common Side Effects
Fatigue: A common side effect of many cancer treatments, including immunotherapy. Patients may experience varying degrees of tiredness and lack of energy.
Skin Reactions: These can include rash, itching, and redness. Skin reactions are often mild but can be bothersome.
Gastrointestinal Issues: Diarrhea, nausea, and vomiting are common gastrointestinal side effects. These symptoms can usually be managed with medication and dietary changes.
Loss of Appetite: Patients may experience a reduced desire to eat, which can lead to weight loss and nutritional deficiencies.
Muscle and Joint Pain: Some patients report pain and stiffness in their muscles and joints, which can affect mobility and quality of life.
Fever and Chills: Flu-like symptoms, including fever and chills, can occur as the immune system responds to treatment.
Serious Side Effects
Severe Allergic Reactions: Although rare, some patients may experience severe allergic reactions, which can be life-threatening. Symptoms can include difficulty breathing, swelling, and anaphylaxis.
Autoimmune Reactions: Immunotherapy can sometimes cause the immune system to attack healthy tissues, leading to conditions such as colitis (inflammation of the colon), hepatitis (inflammation of the liver), and pneumonitis (inflammation of the lungs).
Endocrine Disorders: Immunotherapy can affect hormone-producing glands, leading to conditions such as hypothyroidism or hyperthyroidism.
Kidney Problems: In rare cases, immunotherapy can cause kidney inflammation or damage, which may be detected through changes in blood or urine tests.
Neurological Issues: Some patients may experience neurological side effects, such as neuropathy (nerve pain) or changes in mental status.
Managing the side effects of immunotherapy for ovarian cancer involves a multifaceted approach tailored to the specific symptoms experienced by the patient. Common side effects such as fatigue, skin reactions, and gastrointestinal issues can often be managed with supportive care measures. For fatigue, patients are encouraged to balance rest with light physical activity and maintain a nutritious diet. Skin reactions can be alleviated by keeping the skin clean and moisturized, using mild soaps, and avoiding irritants. Gastrointestinal issues like diarrhea and nausea can be managed by staying hydrated, eating bland foods, and using prescribed medications such as antidiarrheals or antiemetics.
For more severe side effects, such as autoimmune reactions, corticosteroids or other immunosuppressive drugs may be necessary, and treatment may need to be paused or adjusted. Close monitoring by healthcare professionals is crucial to promptly address and mitigate these side effects, ensuring the patient’s safety and improving their quality of life during treatment
Immunotherapy has shown promise in treating ovarian cancer, particularly in advanced stages or recurrent cases. However, the success rate varies among patients, and not all individuals will respond to treatment. Clinical trials continue to explore the efficacy of different immunotherapy approaches.
The latest treatment options for ovarian cancer in 2024 include a combination of traditional therapies (surgery and chemotherapy), targeted therapies (such as PARP inhibitors and angiogenesis inhibitors), and immunotherapies (including immune checkpoint inhibitors and cancer vaccines). Research is ongoing to develop and refine these treatments to improve patient outcomes.
Eligibility for ovarian cancer immunotherapy depends on several factors, including the stage of the cancer, the presence of specific genetic mutations (such as BRCA1 or BRCA2), and the patient’s overall health. Patients with advanced or recurrent ovarian cancer who have not responded to other treatments may be considered for immunotherapy, often as part of a clinical trial.
The response rate to immunotherapy in ovarian cancer patients varies widely. Some studies have reported response rates of around 10-20% for immune checkpoint inhibitors, with higher rates observed in patients with specific genetic markers such as MSI-H or dMMR. Ongoing research aims to identify biomarkers that can predict which patients are most likely to benefit from immunotherapy.
Immunotherapy for Ovarian Cancer: Adjuvant, Combination, and Neoadjuvant – Frontiers in Immunology
Immunotherapy in Ovarian Cancer – Springer
Immunotherapy for Ovarian Cancer – American Cancer Society
Side Effects of Immunotherapy – American Society of Clinical Oncology
Novel Therapeutics in Ovarian Cancer: Expanding the Toolbox – Current Oncology
Ovarian Cancer Immunotherapy and Personalized Medicine – International Journal of Molecular Sciences
Current and future immunotherapy approaches in ovarian cancer – Annals of Translational Medicine
The article is taken from OncoDaily.com
About IMMONC
Immune Oncology Research Institute (IMMONC) is dedicated to advancing research aimed at preventing, treating, and ultimately curing cancer while making these innovations accessible to those who need them. If you're interested in joining our team, please feel free to contact us at [email protected] or at +374-41 310-048.